
If one had to explain it in the simplest terms, humans are practically made of over a hundred trillion microbes. For one human cell, ten microbes are outnumbering it. Most of it resides in the gut of a human being, mostly inside the large intestine.
Microbes such as bacteria, fungi, different viruses, and protozoa that live inside the human body are referred to as microbiome – the genes in the microbes. However, the terms often get used instead of each other.
Studies suggest the microbiome very likely can weigh about 5 pounds. This is because of the total accumulation of genes. If we calculate all the microbes in a human body’s microbiome, it is actually 200 times more than the genes we see in a human genome.
In reality, the microbiome is a recent discovery. It wasn’t until the later part of the 1990s that its existence was acknowledged.
Inside the microbiome, the bacteria perform several tasks. It is useful in digesting our food and keeping the immune system in check, and also offers protection against potentially harmful bacteria that could lead to diseases.
The bacteria inside the microbiome also have a hand in producing vitamins such as thiamine and riboflavin, Vitamin K, and vitamin B12. They directly help with blood coagulation.
Are Microbes Dangerous?
It is a bit of both. Microbes can be extremely good for health. Other than what we mentioned before, they also break down the sugar in the breast milk of a human being. Infants aren’t capable of breaking down the sugar. Instead, they are dependent on the microbes inside one’s gut to take care of the job.
Others have the chance of becoming harmful if they find their way into the wrong parts of the body, or the numbers are higher than what they should be.
What is The Connection Of Microbiome With Health?
For a human body to develop correctly, the microbiome does play an important role. It has a significant effect on the nutrition supply and immunity factors.
The bacteria that exist inside the human body aren’t invaders by any means. Instead, you can refer to them as mutual beneficiaries.
When a person ends up with autoimmune diseases such as multiple sclerosis, fibromyalgia, muscular dystrophy, rheumatoid arthritis, diabetes, and so on, the microbiome is suspected to be dysfunctional. Unfriendly microbes that are more interested in taking from the body than mutually benefiting from it multiply over time in these cases, they alter how the gene acts and disrupt the usual metabolic activities. The result is a dip in the way the immunes system would usually respond to the tissues and other substances inside the human body.
When autoimmune diseases are passed down from family members, it seems to be due to inheriting the microbiome from a family member rather than the DNA.
Where Do Microbes Come From Into The Gut? Do We Just Get Them From Our Surroundings?
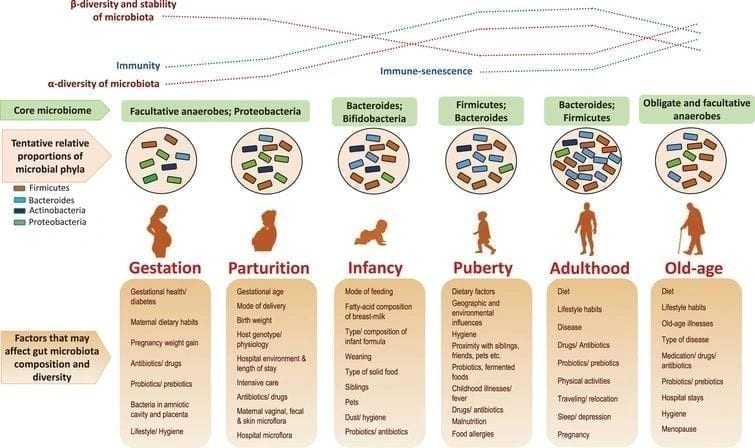
Partially, it can be said to be the case. The general assumption is that when a child is born, as it is making its way through the birth canal, the mother hands over the bacteria to the child. A scientist describes it as similar to gulping while emerging. These primary bacteria are essential for kickstarting the entire process.
It is to be noted that the microbiome level of a mother often shifts a little during pregnancy. Suspected, enough to transfer some to the offspring. What happens if a child is born through cesarean section rather than the natural way then? Well, things are significantly different in that case. Studies suggest this is why children born from the cesarean section seem to be more prone to conditions like type 1 diabetes and asthma. Regardless, doctors don’t recommend attempting to inject microbes into children who are born through cesarean section.
Over the first one or two years, the microbes in our gut go through some changes. At this point, we are being nurtured by breast milk, our immediate environment, and several other factors. By the time a child turns three years old, the gut microbes have already reached stability. However, the situation, along with the stress the human mind and body go through and the drugs a body intakes such as antibiotics, continue to have some effects on microbes while we keep on aging. Ultimately, this means that microbes can change throughout the entire lifespan of a human being.
What is Mycobiome?
When it comes to the human microbiome, though the world has been late in catching up, ultimately, it has been the center of attention of medical research and scientific discovery for years. Researchers mostly focus on the bacterial parts of the microbiota in the human gut.
The focus on the mycobiota in the human gut, which consists of a wide range of fungi species, is a much newer and rapidly developing field of study. The number of fungi is relatively smaller compared to the bacteria.
All recent studies point to one fact – the mycobiome has as much of a part in maintaining humans’ health as the microbiome.
Harmful Effects of Antibiotics
The gut microbiome of a human being is a complex community of sorts that works well on its own. It plays an important part when it comes to dealing with diseases. While the number of microbes varies depending on the human body type, it is integral that a person’s microbiome maintains the same level of bacterial percentage throughout their lifespan.
The gut microbiome has a high chance of being disrupted due to antibiotics medicine. Broad-spectrum antibiotics have more chances of contributing to the disturbance in microbiomes among them. How bad the side effects can get has contributions from multiple factors.
Broad-spectrum Antibiotics
When we talk about broad-spectrum antibiotics, it generally refers to medication that has the range to cover both types of bacteria – gram-positive and gram-negative. Doctors usually administer these antibiotics when a person has already contracted a bacterial infection, and there isn’t much time or resources in hand, but the medicine needs to take effect immediately.
History is proof that broad-spectrum antibiotics have been the savior of uncountable lives. It has also made the field of surgery easier with its advancements and the treatments that have been acquired through it for infections. However, while having excellent uses, broad-spectrum antibiotics also have associations with allergies from outside sources and are the reason resistance towards antibiotics has become popular.
Narrow Spectrum Antibiotics
Narrow spectrum antibiotics are usually made of use when the doctor is confident of the gene or species of bacteria. However, this diagnosis needs to be done in time and as fast as possible before the bacteria have the chance to spread into a full-on harmful infection.
Doctors usually need to have a vast range of experience and training, along with proper resources, to identify the bacterial species so that they can administer the perfect narrow-spectrum antibiotics and at the right time.
The Impact Of Antibiotics On The Microbiome
Human health can take a massive blow when the use of antibiotics becomes too extensive. A large percentage of studies suggest it’s not wrong to blame antibiotics for microbial dysbiosis. An imbalance in the microbiome can lead to inflammatory bowel disease, diabetes, obesity, asthma, and even depression and autism. Some of the adverse effects that antibiotics have on human gut microbiota and the immunity of the human body are:
Antibiotic-Resistant Genes Increase
The health of a host can have a number done on it due to antibiotics. When antibiotics invade the human body, they can lead to an increase in genes that are resistant to antibiotics in the gut microbiome. When antibiotics put pressure on the gut, more sensitive genes will lose while the antibiotic-resistant genes get the chance to grow.
Then, there are three kinds of ways through which antibiotic-resistance genes find themselves in the bacteria. These are transduction, transformation, and conjugation. Many genes are horizontally transmitted among the full range of the bacterial species in the human gut. The antibiotic-resistance genes that are transmitted fall under 6 percent and this is 4.8 times higher than the transmission of antimicrobial peptide-resistance genes.
On top of that, bacterial species accept antibiotic-resistance genes more readily, and this can lead to a lower level of antibiotic-resistance genes for other species in the microbiota of the gut.
Dysfunction of the Immunity System of the Host
It’s not only the gut that gets affected when antibiotic perturbation of the microbes occurs. When microbiota depletes considerably, even the system immunity is severely affected. When microbiota depletes through the administration of antibiotics, it also disables the pulmonary defense system implemented against pathogens. The depletion also results in a noticeable change in metabolism inside the alveolar macrophages.
Metabolites Changes
The immunity of the host is impacted by antibiotics as it alters the bacterial metabolites. It also changes the signal that the host receives from the gut microbiota. The intestinal immune cells and intestinal epithelial cells are affected more than anything due to the change in signal.
As you read through the gut and brain connection section, you will understand how gut bacteria and their imbalance directly affect the brain.
What is the Connection Between the Gut and Brain? What is the Scale of Impact of the Gut on the Brain?
Between your gut and brain is a complicated network of communication, dubbed as the gut-brain axis. The two different organs are connected through biochemical and physical methods.
In your gut, trillions of microbes are heavily involved in the process of making chemicals that affect the working of the brain. The gut microbes are also involved in producing SCFA or short-chain fatty acids. These are propionate, butyrate, and acetate.
The microbes digest fiber, which is how they create SCFA. The SCFA has a hand in affecting brain functions in lots of ways. For one, it can reduce appetite.
One study suggests that when our body consumes propionate, our food intake is affected. That is, we tend to eat less as our brain doesn’t respond to high energy food as a reward as it usually would. The butyrate, another one of the short-chain fatty acids, forms a barrier between the blood and brain. The term for it is the blood-brain barrier.
The microbiome in our gut also creates acids such as amino and bile, which in turn produce chemicals that can affect the brain. While the work of bile acids is usually to absorb dietary fats, they do have some effect on the brain as well.
Some testing on mice has formed the conclusion that under stress and other symptoms of social disorder, gut bacteria produce a lower amount of bile acids, and even the genes involved in the product can get altered.
The gut-brain axis also has deep connections with the immune system.
The human gut and microbes in it control what enters the body and what is excreted out of it, thus maintaining the immune system.
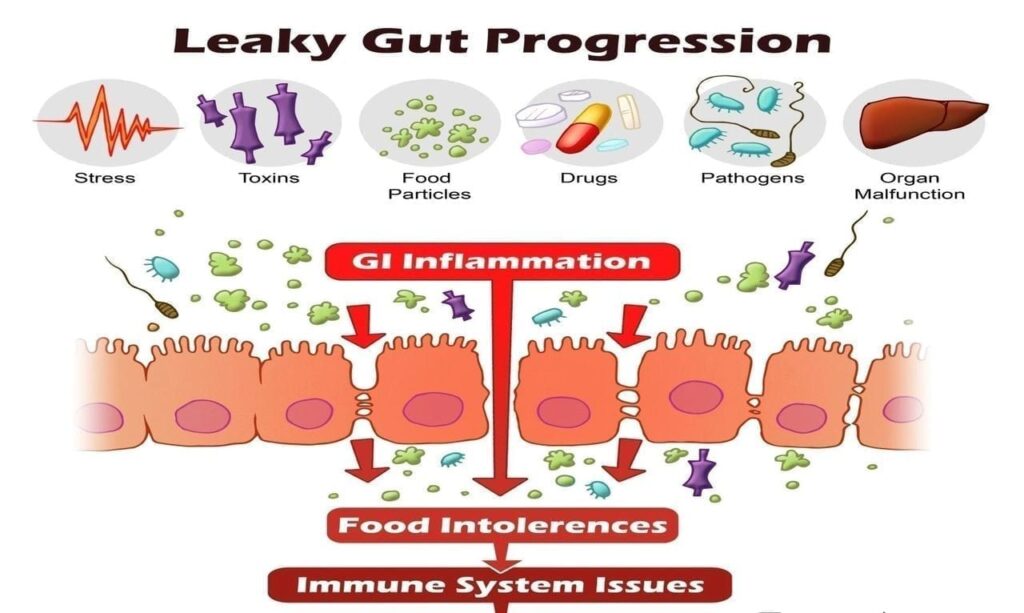
If the immune system is active for too long, there is a chance of it going towards inflammation. Brain disorders such as Alzheimer’s disease and depression all have an association with inflammation. Certain bacteria in our system make Lipopolysaccharide or LPS, an inflammatory toxin. Too much of it accidentally spilling from the gut to the blood, will cause inflammation of the body. This generally happens when the gut barrier is leaky, allowing bacteria and LPS to cross over.
When a person has a high level of LPS in their blood and inflammation, there is a good possibility of them becoming depressed, schizophrenic, or having dementia.
Effect of Probiotics and Prebiotics on the Gut-Brain Axis
If gut bacteria have an impact on brain health, isn’t the logical course of action to change the gut bacteria?
For health benefits, probiotics can be helpful as they are live bacteria. However, all kinds of probiotics can’t be considered the same.
It is psychobiotics, among the probiotics that affect the brain. These probiotics have been linked in improving the anxiety, depression, and stress faced by a person.
When a study was conducted on people suffering from irritable bowel syndrome with either mild or a more generous level of anxiety, the results showed that taking Bifidobacterium longum NCC3001, which is a probiotic, for about six weeks, showed improvement in the symptoms.
Gut bacteria also ferment fibers called prebiotics, which are assumed to affect brain health too. If a person takes galactooligosaccharides, which is prebiotic, for three weeks minimum, the stress hormone in their body reduces significantly. This hormone is called cortisol.
Foods that are good for the gut-brain axis as well.
Fermented Food: Food such as cheese and yogurt have a healthy amount of microbes – lactic acid bacteria being one of them. Studies prove that fermented food has a role in altering brain activities.
Food Containing High Fiber: Fruits, vegetables, and whole grains all have prebiotic fiber that is good for the bacteria in the human gut. Prebiotics has been associated with reducing stress hormones in a person.
Food Containing Omega 3 fats: Omega 3 fat is found in fish that is oily in nature. The human brain also has a high quantity of omega-three fats. After several tests, it has been concluded that the good bacteria in the human gut increases due to omega 3. The chances of developing brain disorders also reduce with the increase in omega 3 fats.
Foods that are rich in Polyphenol: Our gut bacteria devour plant chemicals called polyphenols. As such, in turn, when we consume olive oil, coffee, green tea, or any kind of product with caffeine, we are making our gut bacteria healthier. There has been some evidence in studies that suggests cognition in humans gets a boost too.
Foods That Are Rich in Tryptophan: Tryptophan is a kind of amino acid. It is broken down and converted into what we call serotonin. Serotonin has always been associated with a happy mind, and in turn, better health. For example, cheese, eggs, turkey, contain a high level of tryptophan.
Conclusion
All these studies suggest one thing – whether it is due to long term or short-term antibiotic treatment, the gut microbiome can get permanently disrupted. Once that occurs, the changes in health are long term.
Scientists and doctors alike discourage the use of antibiotics, especially in children and pregnant women. The conclusion is simple, one should not consider antibiotics completely harmless. At the same time, the existence of the microbiome and its entire effect on the human body raises hope that if we could learn to modulate the microbiomes, we would find ways to alter the immunity in our system.
Sources
https://www.healthline.com/nutrition/gut-brain-connection#section4
https://www.taconic.com/taconic-insights/microbiome-and-germ-free/antibiotics-affect-microbiome.html
https://www.nature.com/articles/d42859-019-00019-x
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6511407/
**Disclaimer**
This site and its services are for consumer educational use only. Nothing contained in this article is or should be considered or used as a substitute for medical advice, diagnosis, or treatment. Never start any diet, exercise, or supplement program without consulting your medical provider. This article and its services do not constitute the practice of medicine. Users should always seek the advice of a physician with any questions regarding their health or medical conditions. Never disregard, avoid, or delay obtaining medical advice or following the advice of a physician because of something you have seen or read on this site.




Leave a comment